BONE MARROW TRANSPLANTS
This page provides an overview of bone marrow transplantation, sometimes referred to as haematopoietic cell or stem cell transplantation. It explains terms haematologists use when talking about bone marrow transplantation, its benefits and complications.
WHAT IS A BONE MARROW TRANSPLANT?
A bone marrow transplant (BMT) is a complex treatment procedure for blood diseases and a few autoimmune diseases. In BMT, the patient receives intensive chemotherapy or sometimes radiotherapy followed by administration of bone marrow cells or peripheral blood stem cells that restore the bone marrow function. Surgeons are not involved at any stage during bone marrow transplantation and it is not an operation. It is a complex procedure that usually involves inpatient admission and then outpatient monitoring.
Autologous transplantation, uses the patient’s own whereas allogeneic transplants use cells from a different person. They are more complicated and are therefore used mainly when other therapies have only a low chance of success.
Transplantation is a multidisciplinary procedure involving cooperation of the clinical teams, stem cell collection facility, pharmacy, blood transfusion, stem cell laboratory and in certain cases other centres’ stem cell collection facility. It is a thoroughly regulated treatment and it is only performed in accredited haematology centres.
WHEN WOULD SOMEONE NEED A BONE MARROW TRANSPLANT?
Bone marrow transplantation (BMT) is used for a variety of diseases. These include autoimmune disease such as aplastic anaemia, inherited blood diseases such as sickle cell disease, or malignant diseases of blood system.
Autologous BMT involves a high dose of chemotherapy followed by infusion of the patient’s own cells to help them recover from the side effects. Autologous BMT is mainly recommended for treatment of myeloma and lymphoma. It can also be useful in the treatment of some germ cell tumours and increasingly for some autoimmune diseases such as multiple sclerosis, a disease of the nervous system.
Allogeneic transplants are very different from autologous BMT. They are used mainly in treatment of acute leukaemia – both acute myeloid and acute lymphoblastic. Some patients with lymphoma or chronic leukaemia may also benefit, particularly if they do not respond to other therapies. Myelodysplastic syndromes and aplastic anaemia are other diseases in which allogeneic transplantation plays an important role, particularly in younger patients. Finally, allogeneic transplantation is indicated in some patients with non-malignant blood diseases, including sickle cell disease and thalassaemia.
WHAT HAPPENS DURING THE BONE MARROW TRANSPLANT?
First of all, it is important to discuss the risks and benefits of this therapy and establish if it is reasonable to perform. If autologous transplantation is recommended, it is important to organise stem cell collection.
In case of allogeneic BMT it is important to start looking for appropriate bone marrow or blood stem cell donors. The best donors for allogeneic transplantation are tissue matched family members (most often siblings). If these are not available, an unrelated donor search needs to be undertaken, although in some cases half-matched family donor or occasionally unrelated umbilical cord blood of new-borns may be preferable. Finding the right unrelated donor is sometimes a lengthy process taking several weeks or even months.
Patients need to undergo tests to assess the function of their lungs, heart and other organs and to establish details of their disease. Informed consent needs to be obtained both from patients and from their donors. Subsequently the transplant date is established.
A central line (central venous catheter) is usually inserted to administer conditioning chemotherapy. This is a thin plastic tube leading from its place in the chest, neck or arm to a big (central) vein.
Before transplantation patients receive high dose chemotherapy or sometimes chemotherapy with radiotherapy. This radiotherapy may be total body irradiation or to the main immune tissues. This chemotherapy and/or radiotherapy is called conditioning and is usually given over few days. It will reduce the number of patient’s blood cells in the body in preparation to receive the new cells from the donor.
The bone marrow or stem cells are given after conditioning finishes via a drip (transfused) into a vein, and the cells find their way to home back in the bone marrow. They start working to produce new, healthy blood cells in 2 to 6 weeks, depending on the type of transplant. During this time patients are very susceptible to infection and often require treatment with antibiotics and other anti-infection therapy.
Patients are usually admitted to hospitals for transplants and are nursed in single rooms. They are discharged home after the blood counts recover to a reasonable level. After that outpatient monitoring starts. Full recovery takes approximately 3 months for recipients of autologous transplantation but it is much longer for allogeneic transplant recipients.
HOW ARE STEM CELLS FOR TRANSPLANT OBTAINED?
Stem cells can be harvested from the bone marrow under general anaesthesia in an operation theatre or they can be separated from blood. During autologous transplantation the cells are taken from the patient themselves. In allogeneic transplantation they are obtained from an appropriate, healthy donor.
Bone marrow harvests take cells from the bone marrow of the pelvic bones. This is performed with the bone marrow donor lying flat on their front, under general anaesthesia. A large needle is introduced into the back of the pelvis and liquid bone marrow is drawn using syringes. Repeated suctions are needed to obtain the required amount of bone marrow, which depends on the bone marrow recipient’s weight, but is usually about a litre of bone marrow. The pelvic bone (lower back/upper bottom) is usually painful after this procedure.
However, in most cases stem cells are obtained from the donor’s blood. Normally only very few stem cells leave the bone marrow and circulate in the blood. Growth factors such as G-CSF encourage stem cells to leave the bone marrow and travel to the blood. A course of a few days G-CSF treatment is called stem cell mobilisation. G-CSF is used on its own in healthy donors or in combination with chemotherapy in patients prior to autologous transplantation.
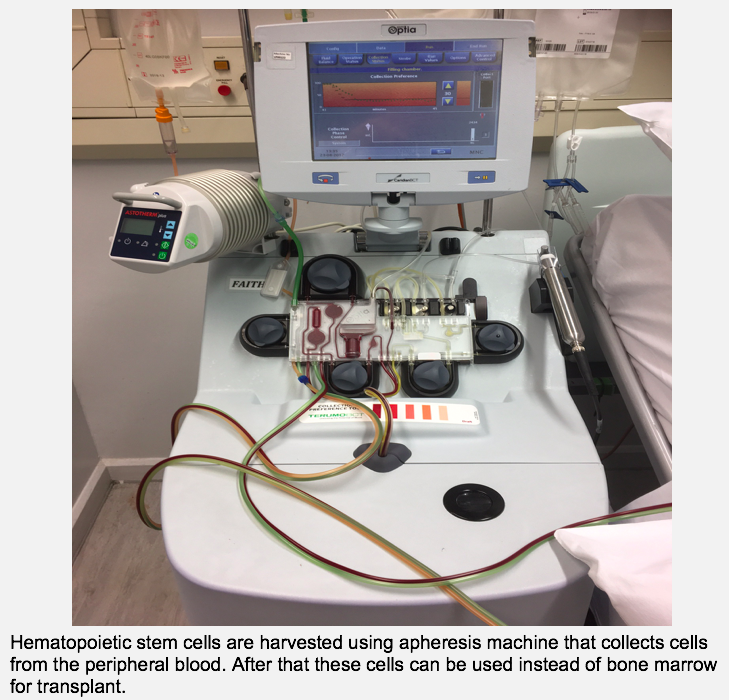
On the last day of mobilisation, stem cells are in the blood in sufficient amounts. They are then collected using an apheresis machine. Blood flows from a vein of one arm to the machine; the stem cells are separated and collected., The rest of blood returns to another vein, usually in the other arm. This is a gentle procedure and it takes only few hours to obtain sufficient amounts of stem cells.
WHAT ARE THE MAIN TYPES OF BONE MARROW TRANSPLANT?
The main two types of transplants are autologous where the patients receive their own bone marrow or stem cells and allogeneic transplants where the cells come from a different person – donor.
AUTOLOGOUS BONE MARROW TRANSPLANTATION
Before an autologous (abbreviated as auto) transplant, stem cells or bone marrow is collected (harvested) from the patient and then it is frozen (cryopreserved). The transplantation itself starts with conditioning. After that the stem cells are thawed and given as an infusion. The control of cancer is dependent on the effect of high dose chemotherapy and/ or radiotherapy which are part of the conditioning. Autologous transplantation is sometimes referred to as high dose therapy with stem cell rescue. Without the stem cell infusion the bone marrow would take a very long time (many months) to recover and this would be dangerous. With infusion of stem cells bone marrow usually recovers quickly, typically 2 weeks after the stem cell infusion in the case of stem cells from blood and within 3 weeks in the case of bone marrow. In essence, autologous stem cells transplantation enables the use of curative high dose chemotherapy, which is otherwise too toxic to give.
Autologous transplantation can cure many diseases where cure would be difficult to achieve other ways, for example lymphoma that returned after initial chemotherapy. It is also used to prolong life when cure is not possible – for example in treatment of multiple myeloma.
ALLOGENEIC BONE MARROW TRANSPLANTATION
Allogeneic transplantation (abbreviated allo) is a complex procedure that requires lots of detailed planning. Post planning the patient is admitted to the hospital and starts conditioning. This contains chemotherapy and/or radiotherapy and immunosuppression. After its completion stem cell are infused and some immunosuppressive drugs continue. The patients immunity becomes very weak for a period of time and they tend to develop infections caused by bacteria, fungi or viruses that would normally not cause any harm to healthy individuals. Most come from patient’s own bodies and are normally harmless. Some bacteria even help with digestion processes, but can cause illness in the context of transplantation. Antimicrobial therapy is often necessary.
Recovery of blood counts usually takes longer than with autologous transplantation. After blood count recovery, the risk of bacterial infections reduces, but it still remains high. Patients are discharged home and intensive day care and/or outpatient follow up starts. Blood tests needs to be monitored and patients remain on a significant amount of medication, usually given by mouth. During this time patients attend hospital relatively frequently, usually once or twice weekly, but the exact frequency depends on their situation. Infections are relatively common so many people need to be admitted to the hospital again during the first 3 to 6 months. After 6 – 9 months the patient’s immunity becomes stronger, so many people are able to start thinking about returning to work. The recovery may be significantly prolonged in the case of significant complications, however.
Allogeneic transplantation is the most potent treatment modality in haematology. It combines chemotherapy and immunotherapy and can cure many diseases not otherwise curable, such as poor risk acute leukaemia, or chronic leukaemia that do not respond to other therapies. However, it also has many potential complications.
WHAT ARE THE MAIN COMPLICATIONS OF BONE MARROW TRANSPLANTS?
Complications of this complex medical procedure can be related to the toxicity of conditioning, which consists of high dose chemotherapy or chemotherapy and radiotherapy. In the case of allogeneic transplantation the patients are also at risk of developing complications related to the immune systems of the patient and the donor as well as toxicity of immunosuppression.
High dose chemotherapy or radiotherapy is associated with same side effects as standard chemotherapy, such as neutropenia, anorexia, nausea, fatigue, hair loss (see chemotherapy), but their intensity may be more pronounced. High doses of chemotherapy are particularly toxic and may damage the lungs, heart or kidneys. This is why these organs are carefully assessed prior to transplantation. Mucositis is damage and inflammation of the lining of mouth, and gut, commonly seen with conditioning. It causes pain in the mouth and ulceration and pain in the abdomen and diarrhoea. All these may be severe requiring intensive treatment with strong analgesia and other drugs. Patients are often unable to swallow and therefore feeding through a tube leading directly to the stomach or directly in a vein may be necessary. The combination of mucositis and low white cell counts (neutropenia) increases the chance of infections. These can develop very fast and lead to sepsis. Prompt investigation and therapy with antibiotics is very important. Occasionally organ support such as the use of a breathing machine or artificial kidney may become necessary. Sadly, sometimes despite all these measures and excellent care patients keep deteriorating and may pass away as a result of these complications. This is referred to as treatment related mortality.
Although any chemotherapy may decrease the chance of being able to conceive a child, this is particularly common with high dose chemotherapy. It is important to discuss fertility issues early during the transplantation planning, and review potential options.
Allogeneic transplants may be also complicated by immune complications. These include susceptibility to infections that results not only from conditioning, but also from administration of immunosuppressive drugs. In addition the new immune system of the donor needs to learn to tolerate the patient’s immune organs and tissues. Graft-versus-host disease results from the new immune system reacting with the patients’ tissues. Most commonly it affects the skin and the gut, resulting in rashes and diarrhoea. Sometimes it may not be easy to diagnose this complication and biopsy samples of affected tissues needs to be analysed in the laboratory. Graft-versus-host disease is initially treated with corticosteroids, often in combination with other immunosuppression. There is therefore an increased risk of infections.
The intent of transplantation is usually to cure the disease. Exceptions to this are autologous transplants for myeloma where we aim to prolong the disease control knowing that the myeloma will recur in future or autologous transplantation for multiple sclerosis where we aim to improve symptoms. Recurrence of disease after transplantation is not unusual. In some cases, more donor cells – lymphocytes can be given to boost further the immune effect of transplantation. The donor’s immunity may be able to retain the control of disease and result in cure, even in disease recurrence after transplant.
For more information about transplantation links: Bloodwise: Seven Steps by Michelle Kenyon
For information on long-term recovery from transplantation see Michelle Kenyon’s and Dr Bronwen Shaw’s booklet The seven steps, the next steps.